
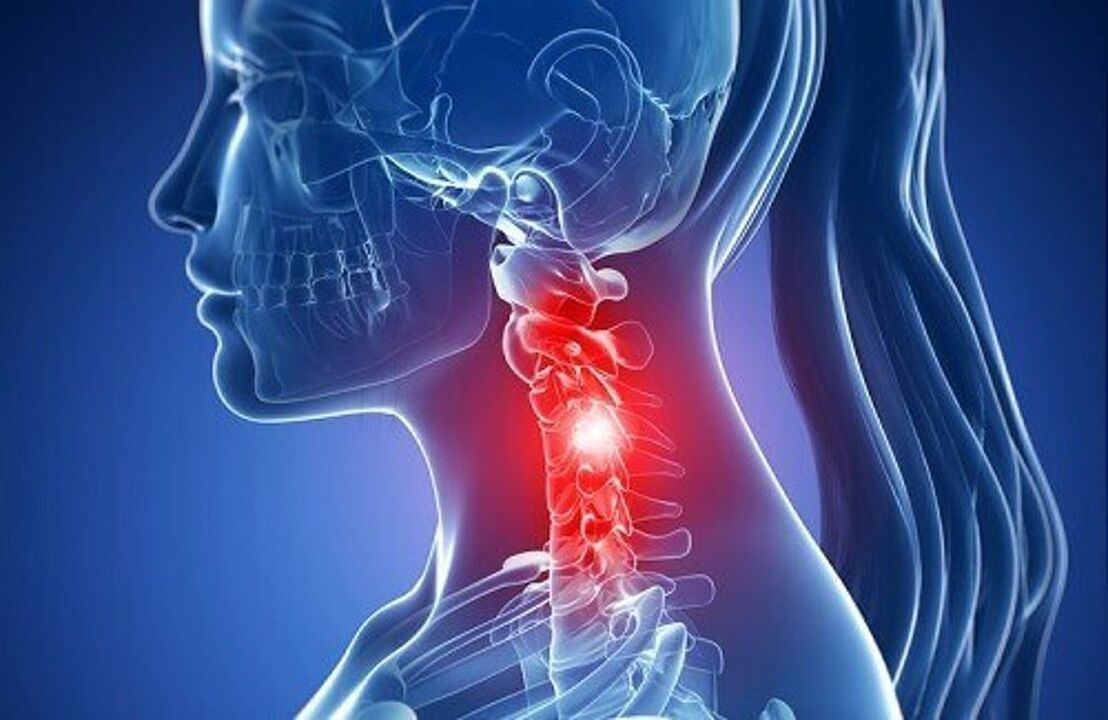
Osteochondrosis is a lesion of the intervertebral discs of a degenerative-dystrophic nature, and the cervical spine is the most vulnerable part of the spine, which has an anatomically different structure of very close adjacent vertebrae and a weak muscular corset. Therefore, even with small additional loads on the neck, a displacement of the vertebrae can occur, which leads to compression of blood vessels and nerves.
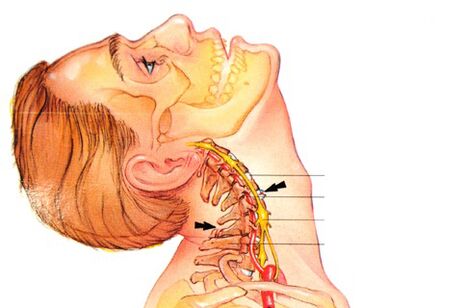
And since the vertebral arteries that are involved in the blood supply to the brain pass through the holes in the transverse processes of the vertebrae in this section, pinching the vertebrae in this section or squeezing the holes from overgrown osteophytes is fraught with very serious consequences.
What's this?
Osteochondrosis of the cervical spine is a progressive polyetiological disease, which manifests itself with the degeneration of the intervertebral discs and the dystrophy of the ligamentous apparatus of the spinal column.
Causes of the event
The main causes and prerequisites for the onset of osteochondrosis of the cervical vertebra are:
- Curvature of the spine, scoliosis.
- Stress, nervous tension negatively affect the general condition of the body, can cause cervical osteochondrosis.
- Postponed infectious diseases often become the main cause.
- Incorrect and uncomfortable body position during sleep (for example, an uncomfortable pillow).
- Congenital problems or the presence of hereditary diseases of the cervical spine.
- Bad posture in youth and adolescence.
- Overweight, obesity of varying degrees. The extra pounds increase the load on the vertebrae and discs, which leads to degenerative processes.
- Back injuries that may have occurred in childhood or adolescence.
- Disruption of metabolic processes.
- Work related to physical work, which can cause diseases of the spine in its various parts.
- Inactive lifestyle, sedentary work, improper performance of any exercise.
For the successful treatment of cervical osteochondrosis, it is first necessary to establish the cause of the event, the prerequisites that provoked its development and eliminate them. Until recently, the disease only occurred in people over the age of 45. Now young people are exposed to it, the age group is 18-25 years old.
Characteristics of the cervical spine
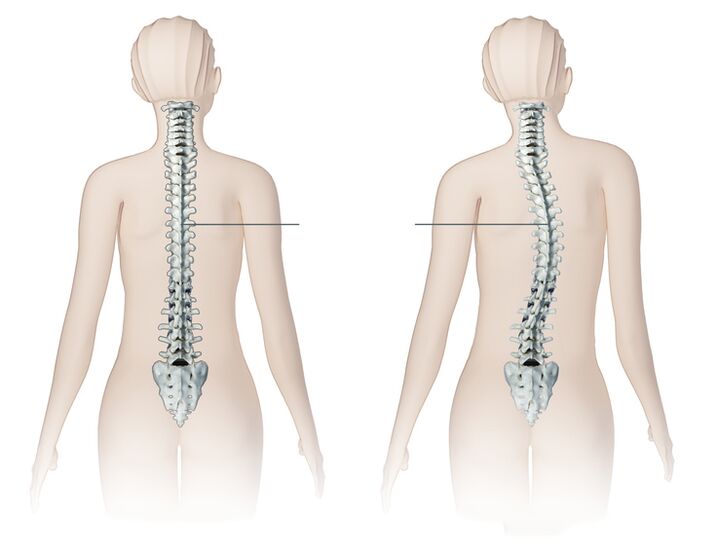
Consider how the cervical region differs from the rest of the spine and that in the process of developing osteochondrosis it is a prerequisite for the development of these syndromes.
- In the cervical region there are important ganglia (nodes) of the autonomic nervous system.
- In the transverse processes of the vertebrae there are holes that form a channel through which the vertebral artery passes, which supplies oxygen and nutrients to the brain, cerebellum, hearing organs, and also to the vertebral nerve. These are the prerequisites for frequent clips of arteries and nerves.
- The cervical spine is the most mobile. It is characterized by all kinds of movements in full. These are the prerequisites for frequent infractions and subluxations!
- The intervertebral foramen of the three lower vertebrae is not round, but triangular. These are the prerequisites for the violation of nerve roots by bone growths, which are formed in osteochondrosis.
- The intervertebral discs are not located between the vertebral bodies along their entire length. In the front, in their place, there are protruding edges of the vertebrae, which are interconnected by joints.
Here are the key characteristics we will start from, analyzing the symptoms and complications of osteochondrosis.
Stages of development
The degree of osteochondrosis is determined by the clinical picture and the patient's complaints. The concept of degree should not be confused with the stages of osteochondrosis. The stages will be discussed below.
- First degree. clinical manifestations are minimal, the patient may complain of low-intensity pain in the cervical spine, it may worsen when turning the head. Physical examination may show slight tension in the neck muscles.
- Second degree. the patient is concerned about pain in the cervical spine, its intensity is much greater, the pain can radiate to the shoulder, arm. Painful sensations increase when tilting and turning the head. The patient may notice a decrease in performance, weakness, headache.
- Third grade. symptoms of cervical osteochondrosis intensify, pain becomes constant with irradiation to the arm or shoulder. Numbness or weakness appears in the muscles of the arm as herniated discs form (see symptoms of a spinal hernia of the lumbar spine). Examination reveals limited mobility in the cervical spine, pain on palpation of the cervical spine.
- Fourth degree. there is a complete destruction of the intervertebral disc and its replacement with connective tissue. Dizziness intensifies, tinnitus appears, impaired coordination.
Symptoms
The severity of the symptoms of cervical osteochondrosis depends on the degree of destruction of the vertebral structures. Symptoms are aggravated by the growth of bone tissue with the formation of osteophytes, radicular syndrome (radicular pain when a nerve is pinched), intervertebral hernia (protrusion of the disc in the spinal canal).
The first signs of the disease are periodic headaches in the occiput, pain in the neck, crunches and clicks in the vertebrae when turning the head, and sometimes a slight tingling sensation in the shoulders. Over time, the symptoms increase and the intensity of the pain increases.
Pain syndrome is the main manifestation of osteochondrosis. Neck pain can be dull, constant, or sharp with lumbago below the occiput when turning the head. The entire cervical region or the projection area of the modified vertebra, as well as the collarbone, shoulder, shoulder blade, and heart area can hurt. Restriction of head movement due to pain often occurs in the morning after sleeping in an uncomfortable position.
The disease leads to compression of the peripheral nerve roots (radicular syndrome) and causes pain along the course of these nerves. Perhaps numbness of the hands or fingers, impaired sensitivity of certain areas of the skin innervated by the pinched nerve.
According to some characteristic symptoms, it can be assumed which vertebrae are affected:
- C1 - violation of sensitivity in the occipital region;
- C2 - pain in the occipital and parietal regions;
- C3 - decreased sensation and pain in the middle of the neck where the spinal nerve has been violated, possible alteration of the sensitivity of the tongue, speech disorders due to loss of control over the tongue;
- C4 - impaired sensitivity and pain in the scapular region of the shoulder, decreased tone of the muscles of the head and neck, possible breathing disorders, pain in the liver and heart;
- C5 - pain and impaired sensitivity in the outer surface of the shoulder;
- C6 - pain extending from the neck to the shoulder blade, forearm, outer surface of the shoulder, radial surface of the forearm to the thumb of the hand;
- C7 - pain spreading from the neck to the shoulder blade, to the back of the shoulder, from the forearm to the II-IV fingers of the hand, impaired sensitivity in this area.
- C8 - pain and sensory disability spread from the neck to the shoulder, from the forearm to the little finger.
Jerking or creaking during neck movements almost always accompany cervical osteochondrosis, which is observed in every patient. The crunch appears during a sharp turn of the head or a backward toss.
Cervical osteochondrosis syndromes
Symptoms of cervical osteochondrosis are grouped together, called syndromes. Their presence and severity may indicate a pathology in the cervical spine with a specific localization.
A group of common syndromes:
- Vegetative-dystonic syndrome. Subluxation of the first vertebra of the cervical spine with displacement can lead to the development of vegetative-vascular dystonia. VSD is not a definitive diagnosis, as it has no pronounced symptoms. There may be neurological signs, symptoms of impaired cerebral blood flow, intracranial pressure spikes, muscle spasms. As a result, the patient's ailments are reduced to dizziness, decreased visual acuity, loss of consciousness, headache and nausea.
- Irritating and thoughtful. Burning and sharp pain in the back of the head and neck, sometimes with a return to the chest and shoulder, which occurs at the time of a change in the position of the head and neck, with sneezing and a sharp rotation of the head.
- Radicular. Otherwise called cervical radiculitis, it combines the symptoms associated with the violation of the nerve roots of the cervical vertebrae. Characterized by "chills" in the affected area, tingling in the fingers, forearms, pasty skin, spread to certain fingers.
- Cardiac. Almost the same picture with angina pectoris often leads to incorrect diagnosis and treatment. The syndrome appears due to irritation of the phrenic nerve receptors, partially capturing the pericardium and the pectoralis major muscle. Therefore, spasms in the heart area are more reflex, as a response to irritation of the cervical nerves.
- Vertebral artery syndrome. It develops directly both with compression of the artery itself, and with irritation of the sympathetic nerve plexus, which is located around it. The pain in this pathology is burning or throbbing in the occipital region with spread to the temples, superciliary arches, crown. It occurs on both one and both sides. Patients usually associate exacerbation with the state after sleeping in a non-physiological position, traveling in transport, walking. With severe symptoms, hearing loss, dizziness, tinnitus, nausea, vomiting, loss of consciousness, increased blood pressure are possible.
Non-specificity and a large number of various symptoms accompanying this disease complicate the diagnosis and further treatment, since some of them can be a sign of completely different diseases.
Diagnostics
As with any diagnosis in medicine, the diagnosis of osteochondrosis is established on the basis of the patient's complaints, anamnesis, clinical examination and auxiliary research methods. X-ray of the cervical spine is performed in frontal and lateral projections, if necessary in special positions (open mouth). At the same time, specialists are interested in the height of the intervertebral discs, the presence of osteophytes.
Of modern research methods, NMR and CT studies are used, which allow more accurate verification of the diagnosis. In addition to the listed methods of further research, it may be necessary to consult related specialists (cardiologist, ophthalmologist, neurosurgeon), and examination by a neurologist is simply vital. A neurologist is engaged in the treatment of osteochondrosis, therefore, after examining the patient, he will prescribe at his discretion the minimum necessary examination.
How to treat osteochondrosis of the cervical spine?
Complex treatment of cervical osteochondrosis can include the following traditional and non-traditional methods: drug treatment, massage, acupressure, manual therapy, physiotherapy, acupuncture, homeopathy, folk remedies, etc.
The main treatment regimen for osteochondrosis is the same for all localizations of this disease:
- First you need to relieve the pain.
- Then the swelling will be removed.
- At this stage, it is necessary to normalize blood circulation.
- Strengthen the muscle corset.
- Improve nutrition and tissue regeneration.
The list of medicines and drugs for the treatment of cervical osteochondrosis at home is very large:
- Anti-inflammatory (steroid). These are hormonal drugs that relieve inflammation and thereby eliminate pain. Most often, for osteochondrosis of the cervical spine, compresses and ointments based on substances of hydrocortisone, prednisolone or dexamethasone are used;
- Analgesics (non-steroidal pain relievers). They are usually prescribed as tablets or capsules. It should be remembered that most of these drugs irritate the lining of the digestive tract. Among the modern drugs used to relieve pain in osteochondrosis;
- Muscle relaxants are drugs that relax muscle tone. They are used in surgery and orthopedics as aids for pain relief. These drugs are administered parenterally, and therefore always under the supervision of a physician. There is a long list of contraindications;
- Chondroprotectors are preparations containing substances that replace the components of cartilage: chondroitin, hyaluronic acid. To achieve a lasting positive effect, such drugs must be taken for a very long time;
- Ointments and gels for external use. This is the most accessible group of drugs for use at home. They are divided into relieving inflammation, warming and pain relievers. Such funds are often advertised. With cervical osteochondrosis, not all ointments are effective, moreover, due to their availability, they are sometimes used unreasonably and without taking into account the peculiarities of pathogenesis.
- Vitamins. With osteochondrosis, vitamins are prescribed that have a beneficial effect on the peripheral nervous system and improve conductivity. Water-soluble vitamins: B1, B6, B12, fat-soluble vitamins: A, C, D, E. In recent years it has become more common to prescribe combination preparations containing both painkillers and vitamin components. An effective preparation consists of B vitamins based on pyridoxine and thiamine, as well as an anesthetic.
Only a team of good specialists can choose the most suitable therapy, which includes neurologist, physiotherapist, masseur, surgeon and vertebral neurologist.
Physiotherapy
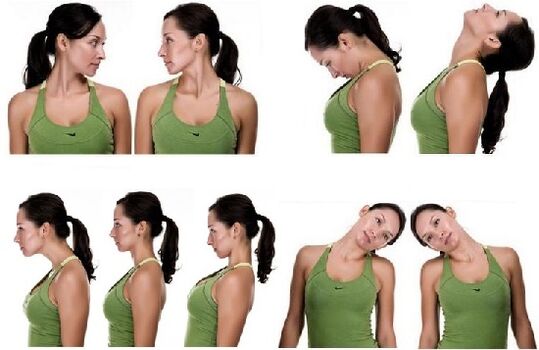
Physical therapy for cervical osteochondrosis should be done outside of the exacerbation. The maximum efficiency of this technique is during the recovery period. There should be no discomfort and pain when performing the complex!
- Exercise n. 1 Lying on your stomach, put your hands on the floor, raise your head and torso, your back should be straight. Stay in this position for 1-2 minutes. Slowly lower yourself to the floor. Repeat 2-3 times.
- Exercise number 2 Lie on your stomach, stretch your arms along the body, turn your head to the left, try to touch the floor with your ear, then turn your head to the right. Repeat 6-7 times in each direction.
- Exercise number 3 In a sitting position, while inhaling, lean forward and try to touch your chest with your head, then exhaling, lean back and tilt your head back. Repeat 10-15 times.
- Exercise n. 4 Sitting down, place your palms on your forehead, apply pressure with your palms to your forehead and your forehead to your palms. Continue this exercise for 30 seconds. Repeat 2-3 times.
- Exercise number 5 Slowly rotate your head first in one direction, then in the other. 10 rotations in each direction. Watch out for dizziness. When it appears, the exercise stops.
Massage therapy
The massage can be performed at home, but very carefully so as not to aggravate and harm the patient. The patient should assume a lying position, put the forehead on the hands and stretch the chin towards the chest. In this case, the neck muscles should be completely relaxed.
- Caress. It is necessary to begin the massage with these movements: stroking the collar area in the direction from the lymph to the supraclavicular and axillary nodes. Then flat, comb-like strokes are applied.
- Lift. To perform push-ups, the massage therapist places a hand on the neck (index and thumb must be together) and moves along the spine. Push-ups can also be done with the edge of the palm up to the shoulder joints.
- shredding. The rubbing serves to warm the muscles, relax them, and improve blood flow to the area. The massage should start from the base of the skull, making circular and straight movements with the fingers. You can also perform saw motions with your palms parallel to your ribs.
- knead. The dough should be done on the neck in a circular motion.
- Vibration. The massage ends with blows and vibrations, which are performed with the help of shaking and beating.

Massage is needed to strengthen muscle tone and relieve pain. Depending on the stage at which osteochondrosis is located, a massage technique is selected. However, during the neck massage, specialists use all the techniques of classic massage: rubbing, stroking, kneading, etc. In cases where the patient has pain in the neck area only on one side, the massage begins in the healthy part of the neck, gradually moving to that part of the neck area where strong painful sensations occur.
Manual therapy
Manual therapy helps to cope with both acute and chronic pain, also increases range of motion and improves posture well. The main methods of manual therapy for osteochondrosis of the cervical spine:

- Relaxing and segmental massage. It is used to warm up the muscles and relieve tension.
- Mobilization. Effects aimed at restoring the functions of the joints. with elongation method.
- Handling. A strong push aimed at the patient's pathological areas. The procedure is accompanied by a characteristic crunch (return of the joint to its normal position).
A specialist who practices manual therapy should be fluent in these techniques. Otherwise, any mistake can cause injury.
Orthopedic pillows

Orthopedic sleeping pillows are an effective preventative measure. In many cases, osteochondrosis is aggravated by further compression of the cervical artery and nerve roots while sleeping on an uncomfortable pillow. The orthopedic product ensures a uniform horizontal position of a person during sleep and thus ensures a physiologically adequate blood supply to the brain.
When choosing a pillow, the individual anatomical characteristics of a person should be taken into account and correlated with the volume and characteristics of the filler. A properly selected pillow brings tangible benefits to a patient with osteochondrosis of the cervical spine.
Physiotherapy
Physiotherapy procedures for cervical osteochondrosis:

- Electrophoresis. It should be used with pain relievers (anesthetics), which are injected under the skin by means of electronic pulses
- Ultrasound. It has a beneficial effect on metabolic processes in the tissues of the cervical spine, thanks to which swelling is removed, pains disappear.
- Magnetotherapy. A safe method of treatment, which consists of exposing damaged cells to a low-frequency magnetic field. Gives an analgesic effect, acts as an anti-inflammatory agent
- Laser therapy. Improve blood circulation in the affected area, relieve tissue swelling, pain.
Physiotherapy procedures have a beneficial effect on discs and vertebrae in cervical osteochondrosis. In combination with taking medications, the combined treatment helps to get rid of the symptoms of the disease. The procedures are performed in a hospital or in specialized offices at polyclinics. Before starting the course, you need to consult a doctor, determine the duration of physiotherapy, types. It is strictly forbidden to pass it during an exacerbation.
shants collar

The Shants Collar is a soft and comfortable device that attaches with Velcro to the back and is used for cervical osteochondrosis. But not for treatment, but for temporary relaxation and fatigue relief. It cannot be worn without taking it off, otherwise the neck muscles will stop working and will soon atrophy. If the Shants collar is selected correctly, the patient feels comfortable and protected.
The collar is selected strictly according to the size in the pharmacy or orthopedic store. Better in the store, because the people who work there, as a rule, know their business and product features quite well, which means they can help in each specific case.
Folk remedies
If the pain of osteochondrosis of the spine becomes unbearable and regular, then you will accept anything to stop it, and here the traditional complex treatment will be successfully supplemented with alternative methods.
- insist on celery root (5 grams per 1 liter of boiling water) for 4 hours, drink one tablespoon before each meal;
- honey compress, for which we take 2 tsp. honey and 1 mummy tablet. We heat the components in a water bath, spread them on a cloth and apply them on the cervical region, ie the neck, at night;
- in case of acute pain, the cultivation of horseradish in the countryside helps me. I just wash its leaf, pour it with boiling water, cool it a little, apply it to the neck and wrap it with a thin scarf for the night - in the morning you can already live and work;
- we insist on chamomile flowers in vegetable oil for two days, preheating to a boil (for 500 ml of oil you need 30 grams of plant), rub into the painful areas;
- The potato and honey compress also helps, for this, the root crop must be grated and mixed with honey in the same amount, applied to a large neck overnight, used regularly, at least once a week.
Prophylaxis
As usual, proper prophylaxis will help to avoid osteochondrosis of the cervical spine, but, of course, all physical exercises must be performed regularly, otherwise there will not be much benefit from "periodic" exercises.
It remains to remember simple rules:
- eat more foods with a lot of calcium and magnesium. These are fish, peas, legumes, nuts, cheese, herbs, but it is better to refrain from sugar, flour, smoked and spicy foods.
- regularly practicing sports, in particular swimming, water aerobics, gymnastics for stretching and flexibility of the vertebrae is also suitable for preventing osteochondrosis, which can be practiced at home.
- during sedentary work, at least a couple of times a day, perform a special set of exercises, an example of which is in the video.
- choose a good orthopedic mattress and an ideal neck pillow, supporting your head in a dream in the correct anatomical position (yes, your favorite huge feather pillows will not go away with spinal problems! ).
If you already have such a diagnosis, the patient should spare the spine, namely:
- Be very careful with lifting and carrying weights, it is better to go to the store twice than to pull heavy bags with both hands, incredibly straining the neck and shoulder girdle;
- Do not overcool, avoid drafts and the flow of cold air from the air conditioner (some people like to cool off on a hot day, standing with their backs to the fan);
- When you bend your body forward, it remembers osteochondrosis;
- Avoid local overheating of the muscles, which can happen to those who love an excessively hot bath;
- Do not forget to periodically detach yourself from the monitor, change the position of the body, do not sit for hours or even days;
- Rest the neck, for which you need to purchase a Shants collar;
- If possible, if the state of the cardiovascular system allows, take a steam bath.
In conclusion, I would like to say that a child threatened with osteochondrosis (the father and mother already have it) and an adult who acquired the disease in the course of life are simply obliged to take preventive measures in order not to become disabled and not to be on the operating table, because this operation is quite difficult and requires long-term rehabilitation. It is also not always possible, because there are inoperable cases, so it is better to protect health from a young age, as long as the discs are intact and unnecessary growths do not compress blood vessels.



















